Ways to prevent the spread of infection caused by CoVID-19 in Clinical Laboratories
These days, the concern of the World Health Organization and many Health centers is that the spread of the new Cov-2 coronavirus may be dangerous for healthcare personnel, especially diagnostic laboratory staff.
Therefore, the researchers of the COVID-19 Working Group of the International Federation of Clinical Chemistry and Medical Laboratory (IFCC) have published a review article that containing a set of recommendations which are adapted from official documents of international and national health organizations, on the level of biosafety and routine clinical laboratory procedures.
A biosafety measures for routine clinical chemistry laboratories that operate at biosafety levels 1 (BSL-1; work with agents posing minimal threat to laboratory workers) and 2 (BSL-2; work with agents associated with human disease which pose moderate hazard).
Coronavirus 2019 (COVID-19) is the third most common type of coronavirus outbreak in the last 20 years, after acute respiratory syndrome (SARS) and Middle East Respiratory Syndrome (MERS).
But unlike the previous two cases, COVID-19 spread rapidly around the world and has infected more than 3 million people so far. The virus, which has killed more than 200,000 people, has been identified by the World Health Organization (WHO) as It was called the “global pandemic.”
Meanwhile, one of the concerns of health organizations around the world is that the outbreak of the new coronavirus may be dangerous for health care personnel and diagnostic centers staff.
Although initial reports have delineated this new infectious disease as being less severe than SARS, recent epidemiologic data of the WHO attests that the worldwide death rate due to COVID-19 is progressively increasing, approximating that of SARS (i.e. 6.86% vs. 9.56%), especially in certain countries like Italy (13.53%) and Spain (11.07%).
Researchers say the above-mentioned figures, along with the rapid spread of the infection, have increased the likelihood of staff shortages in treatment and diagnosis. Therefore, it is necessary to prepare and provide guidance on the use of appropriate safety methods to protect the personnel of the medical staff as well as the personnel of the diagnostic department more than before.
Characteristics of the virus
COVID-19 is caused by a virus belonging to the coronaviridae family, named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) by the International Committee on Taxonomy of Viruses. SARS-CoV-2 is a single-stranded RNA virus, with RNA genome size of approximately 30,000 bases and viral particle size comprised between 70 and 90 nm.
It is now acknowledged that the virus binds to angiotensin-converting enzyme 2 (ACE2), a transmembrane enzyme which plays a central role in the renin-angiotensin-aldosterone system (RAAS).
Recent evidence has been provided that ACE2 is widely expressed in human tissues and organs, especially in cells of the higher and lower respiratory tracts (especially alveolar epithelial cells), heart, kidney, esophagus, intestine, as well as in lymphocytes.
Route of transmission of SARS-CoV-2
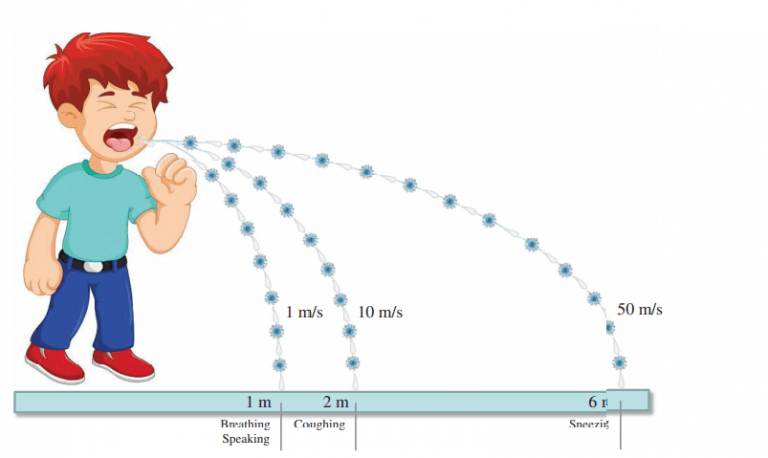
SARS-CoV-2 can usually be transmitted through large airborne particles (approximately 5 μm in diameter) instead of small aerosols, as well as from contaminated hands and surfaces.
According to the latest evidence provided by the WHO and the US Centers for Disease Control and Prevention (CDC), SARS-CoV-2 is mainly spread through large respiratory droplets through sneezing or coughing in patients with CoVID-19. It then reaches another person’s nose, mouth, or eyes, or is inhaled, transmitting it to humans.
Although most large respiratory droplets containing SARS-CoV-2 would fall to a surface within a distance of approximately 1 m (i.e. ~3 feet) during normal breathing, as they are conveyed by exhaled air at a speed of approximately 1 m/s, coughing or sneezing may considerably enhance propagation velocity (i.e. 10 m/s for coughing and 50 m/s for sneezing, respectively), as well as the corresponding propagation distance of these droplets (i.e. 2 m for coughing and 6 m for sneezing, respectively).
The following recommendations are based on studies and observations of what was learned in the early epidemics of SARS and MERS. Therefore, depending on the rate of change of B symptoms and the CoVID-19 relief process and the emergence of new information, the recommendations presented in this article may change over time.
What personal hygiene and personal protective equipment (PPE) should be used in clinical chemistry laboratories during the COVID-19 pandemic?
With respect to sample transportation, it is recommended that all conventional laboratory specimens (blood, urine, respiratory, feces and so forth) be tightly capped and transported to the laboratory in biohazard zip-locked bags, within a leakproof cryobox with a clearly visible biohazard label.
In terms of personal protective equipment (PPE) it is necessary for laboratory staff to maintain safety in the laboratory during the Corona period by useing personal protective equipment (PPE) such as gan, laboratory cover, long cover on shoes, gloves (preferably made of nitrile or latex without Powder), use N95 mask, safety goggles (or Gagel) and face shield. Recommendations for laboratory coatings depend on the type of activity.
Laboratory staff can reduce the possibility of being infected with the virus by following standard safety tips (such as washing your hands regularly with soap and water for at least 40 seconds or using standard disinfectants if you don’t have access to hand washing and avoiding touching your face). .
The use of this equipment also requires the following points:
- It is better to use 2 gloves (first short leg gloves and then long leg gloves) considering the high risk.
- It is important to note that the use of N95 masks is required during experiments in which high aerosol formation is likely, such as the process of centrifugation of the sample, mixing or mixing of the sample, and so on.
- Laboratories must also take into account the fact that in order to observe the safety tips in the laboratory during the Corona period, it is necessary that the personal protective equipment has the desired quality and is provided in different sizes and appropriate for the staff.
- Observing the order of wearing and removing personal protective equipment is also of particular importance in maintaining the safety and health of employees.
How should laboratory staff handle routine patient specimens during the COVID-19 pandemic?
Laboratories even need to use automated devices with closed compartments to routinely examine body fluids such as blood, urine, and so on.
Samples should also be placed in a special container immediately after the test run and samples should be disinfected or autoclaved quickly.
When manual laboratory techniques are used for processing specimens and there is a risk of generating aerosols, samples with safety caps should be centrifuged in sealed rotors with a lid on. Consider the min/max filling volume of vessels. Do not exceed the vessel speed limit. Use plastic vessels instead of glass, which are more likely to break or leak. Alternatively, open and load/unload the rotor in a biosafety cabinet.
If a tube breaks or leaks, wait for 30 min before opening the centrifuge or aerosol-tight lid or cap to let the aerosols settle. Further manual processing such as opening tubes, jars, pipetting, aliquoting, diluting, vortexing and extracting specimens should be handled in a BSL 2 cabinet to avoid contamination during performance of aerosol-producing activities in samples potentially containing SARS-CoV-2 particles.
If an accident is suspected, or in some way the centrifugation is abnormal, stop the centrifugation. After replacing the biosafety level 3 protection equipment, stop centrifugation for more than 30 min, carefully open the lid, and spray and sterilize with 75% ethanol or other disinfectants. Take out the centrifuge rotor with blood collection tubes and then put them in the biosafety cabinet to treat.
How should staff decontaminate laboratory equipment and surfaces during the COVID-19 pandemic?
SARS-CoV-2 is a coated virus, and the outer layer of coated viruses is often relatively easily damaged by common environmental disinfectants and the causative agent of CoVID-19 disease is eliminated.
Most studies have shown that standard disinfection processes and the use of solutions containing 70% alcohol, or freshly diluted household bleach (including products containing sodium hypochlorite); 5-min incubation of a virus culture with various disinfectants, including 1:50 household bleach, 60%–70% ethanol, up to 7.5% povidone-iodine, over 0.05% chloroxylenol or chlorhexidine and 0.2%–0.4% benzalkonium chloride, has killed the virus.
Laboratory staff should disinfect work surfaces with standardized and effective disinfectants for SARS-CoV-2 infections, depending on their workload, but the interval between each disinfection step should not exceed 3 hours.
The best thing that labs can do in this situation is to increase awareness of the safety issues in the laboratory during the Corona era. You should consider this as an opportunity to learn about ways to prevent laboratory injuries and damage. The epidemic will be eradicated one day, but the lessons learned and the laboratory’s safety improvement opportunities will continue until later years.