the Interpreting Diagnostic Tests for SARS-CoV-2
Recently an article has been published on JAMA (general medical journal) about the Interpreting Diagnostic Tests for SARS-CoV-2.
The article outlines how to interpret two of the most commonly used diagnostic tests, Reverse Transcriptase-Polymerase Chain Reaction (RT-PCR), and IgM & IgG Enzyme-Linked Immunosorbent Assay (ELISA); in detecting ‘severe acute respiratory syndrome coronavirus (SARS-COV-2)’, in CoVID-19 infected adults, who are not immunocompromised.
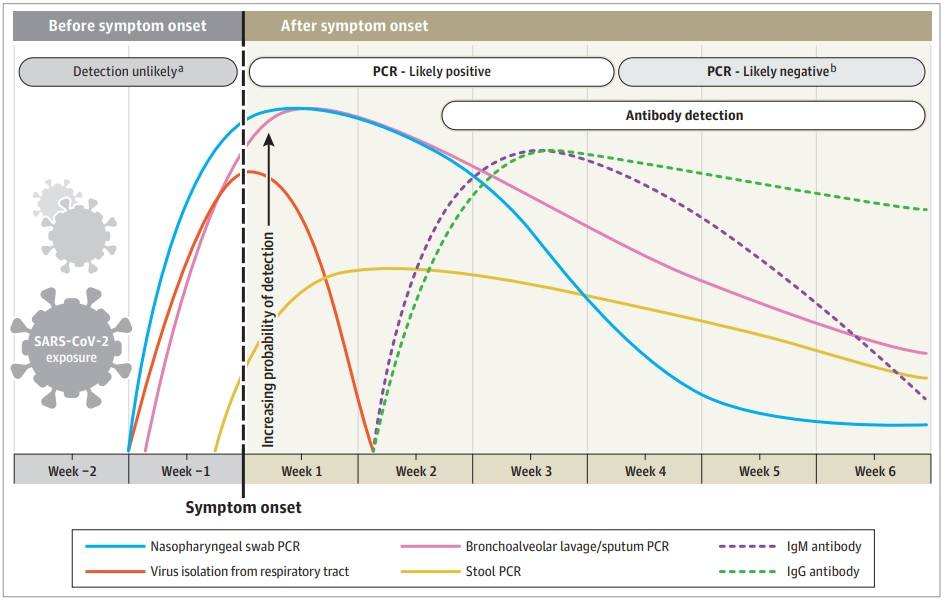
RT-PCR diagnostic tests are the most commonly used at this point, and have 100% specificity; they work by targeting one or more of the virus’s RNA genes from sample specimens of the upper respiratory tract of infected individuals. Using RT-PCR, viral RNA is detected (PCR positive) on the first day and peaks during the first week of symptom onset, PCR positive results decline during the third week of symptom onset, and become undetected in later weeks. A PCR positive result is not a conclusive indicator for the presence of viable virus, it just detects viral RNA. False positives in RT-PCR tests are attributed to reagent contamination and technical errors.
There has been viral RNA detection in certain infected cases that are outside the normal findings, (RT-PCR positive result beyond week 6 of the initial positive result; a positive result after 2 consecutive negative results a day from each other), and there have been no conclusive findings to explain such anomalies. The timeline of a positive PRC result varies between specimen types; in sputum, PRC positivity declines much slower in-comparison to a nasopharyngeal swab, thus positive PCR results can be detected in sputum samples after the nasopharyngeal swab tested negative; stool can test PRC positive 4-11 days post a PRC negative nasopharyngeal swab without any relevant clinical severity.
The second diagnostic test for SARS-CoV-2 is serological diagnosis. This test detects CoVID-19 indirectly by measuring the host’s IgM and IgG antibodies. The study population for this diagnostic method are individuals who are immune, and potentially protected from the virus. IgG and IgM ELISA can be positive 4 days post symptom onset, however, IgM and IgG antibody detection peaks at weeks 3.
Figure Summary:
In summary, viral detection is unlikely during week 1 and week 2 before symptom onset. The probability of viral detection increases for RT-PCR tests during weeks 1& 2 (and to a lesser extent week 3) after onset of symptoms, and declines from week 3 onwards, where PCR negative results are more likely (PCR of a nasopharyngeal swab). Antibody detection begins at the end of week 2 post symptom onset; IgG detection peaks at week 3 and slightly declines overtime; whereas, IgM detection peaks at around the same time as IgG, however detection declines much quicker than IgG at weeks 5, and disappears by week 7.