Black Fungus and CoVID 19; Rumors and facts
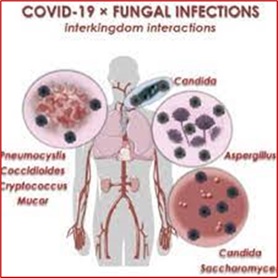
In India, the widespread outbreak of CoVID19 has led to an increase in cases of a deadly fungal infection called mucormycosis, known as “black fungus”. The infection is as dangerous as the media portrays it, but there are various rumors about the source of its spread and treatment on social media, each of which should be thoroughly investigated instead. People with severe CoVID19, like those in ICU wards, are vulnerable to bacterial and fungal infections. The most common fungal infections in patients with CoVID19 include aspergillosis or invasive candidiasis or mucormycosis (black fungus).
What can mucormycosis have to do with CoVID-19?
The human body is not the usual habitat for fungi belonging to the order Mucorales, such as Mucormycosis, which includes species commonly found in soil, dust, decomposing vegetation, and animal manure. Our immune system usually resists fungi and prevents them from growing, but as we said, having a disease or health problem such as diabetes, CoVID-19 and a variety of steroid treatments can weaken the human immune system to such an extent that these microorganisms in the body As a suitable place for their growth.
Diabetes, for example, not only increases the risk of CoVID19 but also provides the body with a breeding ground for a variety of fungal infections. Worse, note that both CoVID19 and the steroid dexamethasone, used by intensive care physicians to treat patients with coronary artery disease, suppress immunity.
What is mucormycosis or black fungus?
Mucormycosis (formerly called zygomycosis) is a serious fungal infection that can live throughout the environment. Mucormycosis mainly affects people who have health problems or are taking medications that reduce their body’s ability to fight germs and disease. The disease usually affects the sinuses or lungs after inhaling fungal spores from the air. It can also occur after cuts, burns, or other skin damage.
Types of mucormycosis and their symptoms
- Rhinocerebral mucormycosis (sinus and brain) is an infection of the sinuses that can spread to the brain. This type of mucormycosis is more common in uncontrolled diabetics and in people with kidney transplants. Symptoms include unilateral swelling of the face, headache, nasal or sinus congestion, blackheads on the nose or upper mouth, and fever.
- Pulmonary mucormycosis is the most common type of mucormycosis in people with cancer and in people who have had an organ transplant or a stem cell transplant. Fever, shortness of breath, cough, and chest pain are symptoms.
- Gastrointestinal mucormycosis is more common in young children than adults, especially premature and low birth weight infants who are less than 1 month old and need antibiotics, surgery, or steroid medications that reduce the body’s ability to fight germs and disease.
- Cutaneous mucormycosis after the fungus enters the body by scratching the skin (for example, after surgery, burns, or other skin injuries). This is the most common form of mucormycosis among people who do not have a weak immune system. Symptoms of cutaneous mucormycosis can appear as blisters or sores, and the infected area may become black. Abdominal pain, vomiting, and abdominal bleeding are symptoms.
- Disseminated mucormycosis occurs when the infection spreads through the bloodstream and affects another part of the body. This infection usually affects the brain, but can also affect other organs such as the spleen, heart, and skin, which is why it is considered an opportunistic infection.
Some of the symptoms mentioned above may be the same between mucormycosis and the Covitine storm caused by CoVID19. It should be noted that cytokine storms are a physiological response in humans and other animals in which the innate immune system causes uncontrolled release and overproduction of pro-inflammatory signaling molecules called cytokines.
On May 26, 2021, 11717 cases of mucormycosis were confirmed in India, which has more diabetics than any other country in the world except China, and this has a huge impact on the high number of patients with black fungus in this It has country. Even before the Corona epidemic, the prevalence of mucormycosis in India was 70 times higher than in the rest of the world.
Why is Mucormycosis called black fungus?
This fungus disrupts blood circulation to the infected tissues and causes people to change their skin color to black, hence the term “black fungus”; But it should be noted that this name does not mean that the color of this type of mushroom is black. Professor Malcolm Richardson, a professor of medical mycology at the University of Manchester, UK told Medical News Today that the name was “completely inappropriate” for this type of fungal disease.
“The causative agents of mucormycosis, for example, Rhizopus oryzae, are hyaline (transparent),” he wrote in an email.
“From a mycological point of view, the term ‘black fungus’ (or black yeast) is limited to fungi called dermatoses that have melanin in their cell walls. Many people have tried to correct this on Twitter, but to no avail. “.
He said the media in India used other misleading terms called “white fungus” and “yellow fungus” to describe types of mucormycosis.
Rumors about the transmission of mucormycosis
There are several theories about the source of mucormycosis infections on social media, many of which are baseless.
- Person-to-person transfer
Mucormycosis cannot be passed from person to person, so there is no need to isolate infected people from other patients unless they also have CoVID19 at the same time.
- Fungi that grow in water, oxygen capsules, or humidifiers
Some media experts have concluded that fungi may grow in dirty water, in-hospital oxygen cylinders, or humidifiers; However, there is no evidence of this, and mycologists have pointed out that fungi cannot produce spores in liquids.
- Facial masks contain black fungus
This is just a rumor; There is no evidence that face masks can shelter fungi and make them grow.

Black fungal disease mortality rate before and after the CoVID-19 epidemic
Without immediate treatment with antifungal drugs and surgery to remove necrotic tissue (dead tissue from this type of fungal disease), mucormycosis is often fatal. Prior to the CoVID19 virus epidemic, the Centers for Disease Control and Prevention (CDC) reported an overall mortality rate of 54%, according to credible sources.
In a systematic review from 2021, all cases of CoVID19 infected with black fungus have been reported in scientific sources, of which 82 are in India and 19 in other parts of the world. Among these cases, the fatal black fungal disease has been reported in 31%.
Dr. Awadhesh Kumar Singh and colleagues report that about 60% of all cases of black fungus occur during active infection with the coronavirus, and 40% develop after recovery. . In total, 80% of patients also had diabetes and 76% of them were treated with corticosteroids.
How is mucormycosis diagnosed?
When diagnosing mucormycosis, health centers consider a person’s medical history, symptoms, physical examinations, and laboratory tests, and use standard and common methods to diagnose it. Also, in cases where specific diagnostic equipment and tools are available based on the DNA of the fungal pathogen, molecular methods can be used to detect different molecular targets, including genes of ribosomal DNA protection and genes of variable regions of the Internal Transcribed Spacer (ITS). Provides interspecific resolution, the most common methods of molecular detection (PCR tests) for fungi.
Health centers that suspect a person has Mucormycosis in the lungs or sinuses should collect a sample of fluid from the respiratory system and send it to a lab for laboratory diagnosis. Tissue biopsy may also be performed, in which a small sample of damaged tissue is analyzed in the laboratory to prove mucormycosis under a microscope or in a fungal culture medium.
As mentioned earlier, these days, with the penetration of molecular biology techniques into diagnostic fields, it is possible to completely cure the patient by rapidly diagnosing the cause of the infection, and using molecular methods to diagnose is one of the best methods. In addition to performing clinical diagnostic tests, you may need imaging tests such as CT scans of your lungs, sinuses, or other parts of your body, depending on the location of the suspected infection.
Treatment of mucormycosis
Mucormycosis is a serious infection that requires treatment with prescribed antifungal drugs, usually amphotericin B, posaconazole, or isoconazole. Some are given intravenously and some by mouth. Other drugs, such as fluconazole, voriconazole, and echinocandins, are not effective against the fungi that cause mucormycosis. Often, advanced mucormycosis requires surgery to cut the infected tissue.
Pulmonary aspergillosis and invasive candidiasis associated with CoVID19
Scientists are still investigating aspergillosis (infections caused by the fungus Aspergillus) in people with severe CoVID19. In the past, scientists thought that aspergillosis occurred almost entirely in people whose immune systems were severely weakened. However, aspergillosis has been increasingly reported in patients without a weakened immune system but with severe respiratory infections caused by viruses, including the flu.
Patients admitted to Covid19 are at risk for opportunistic infections associated with health care facilities, including candidiasis or Candida-induced circulatory infections. Early detection and control of Candida infections and drug-resistant infections is key to reducing death from Quid 19 in patients with severe fungal infections and CoVID19.
References:
- https://www.medicalnewstoday.com/articles/black-fungus-and-covid-19-myths-and-facts
- https://indianexpress.com/article/lifestyle/health/mucormycosis-why-are-covid-19-patients-being-affected-by-black-fungus-7321627/
- https://www.cdc.gov/fungal/diseases/mucormycosis/index.html
- https://www.cdc.gov/fungal/covid-fungal.html
- https://wwwnc.cdc.gov/eid/article/27/5/20-4412_article