HPV/human papillomavirus; From epidemiology to diagnosis
Introduction:
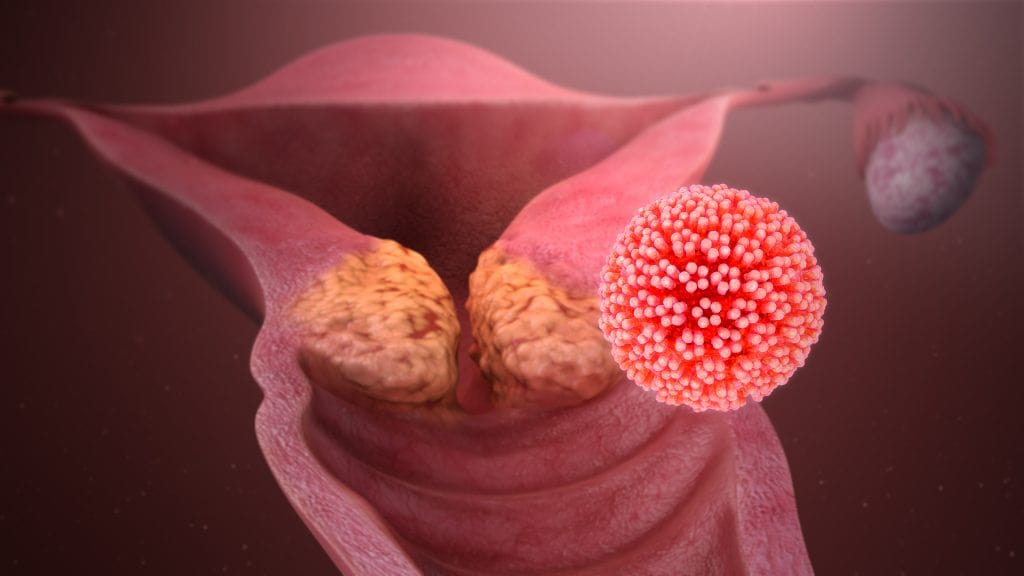
Papillomavirus or human papillomavirus (HPV) is a double-stranded DNA virus belonging to the papillomavirus family and is considered one of the most important causes of sexually transmitted diseases (STDs). Some of these warts are not related to sexual intercourse and can appear like warts on the hands and feet or in the genital areas, which leads to its sexual transmission (of course, in people who have relationships outside of the active framework in terms of sexual activity). This virus has a wide genetic diversity and about 150 genotypes have been identified.
Some of its genotypes can cause cervical cancer, and these genotypes are called high risk, and others that do not cause cervical cancer are called low risk.
Most of the patients have no clinical symptoms and a high percentage is cleared by the body’s immune system. The most important high risk genotypes include the two genotypes 16 and 18, which are mainly related to the occurrence of cancer in the genital area, of course, they also lead to genital warts, and the two genotypes 6 and 11 are the most important low risk genotypes, which lead to the occurrence of wart lesions in the genital area. The body and genital areas are different in both sexes.
Prevention:
Like most infectious and especially viral diseases, prevention is much more beneficial than treatment, and for this purpose, fortunately, several types of vaccines are available in the world:
- Ceravrix is a divalent vaccine or bivalent vaccine (2vHPV) that protects against two high-risk genotypes 16 and 18.
- Gardasil quadrivalent or tetravalent (4vHPV) Gardasil vaccine that protects against 4 genotypes 6, 11, 16, and 18.
- The 9-valent Gardasil vaccine, Gardasil 9 is a so-called 9-valent (9vHPV) vaccine that provides immunity against 9 genotypes 6, 11, 16, 18, 31, 33, 45, 52, 58.
Two types 16 and 18 have been detected in about 66% of all cervical cancers, and two types 6 and 11 have been detected in over 90% of genital warts.
Note: The vaccine is not recommended for pregnant women.
The vaccine can be prescribed regardless of the history of genital warts or the results of the HPV test and Pap smear test.
It is said that it is better to vaccinate children under the age of 19.

Diagnostic considerations:
Different HPV diagnostic methods are used to detect different genotypes, especially to check the presence or absence of high-risk genotypes, as well as to follow up treatment conditions or in women who have unusual cytology and histology tests.
Important things that people with HPV infection should know:
- Genital infections are common. Many people who are sexually active may be infected but do not experience clinical symptoms.
- Having an HPV infection does not necessarily mean that a person has an unusual sexual relationship.
- Many HPV infections clear up on their own.
- Genital warts or other infections of the genital area, if chronic, may cause cancer in different parts of the genital system.
- Smoking cessation counseling is considered an important issue because it is an effective factor in the occurrence of cancer and helping in its development.
- Genotypes that cause warts are different from those that cause cancer.
- Infected pregnant women who have an infected genital tract may transmit the infection to their babies. There is a possibility of transmission in different sexual contacts between men and women in different ways if the genital area is infected and the contact is not protected.
- HPV infection itself does not make it difficult for a woman to get pregnant or continue pregnancy, but the surgical methods that are considered for treatment make this process difficult.
- Using protective equipment such as condoms reduces the chance of infection. But the parts that are not covered by the condom still have a chance of infection, so the condom does not offer 100% protection.
Diagnostic methods:
Among the diagnostic methods, we can refer to the Pap smear test method, which is performed by a doctor during the physical examination of a sample from the cervix, which, of course, has limitations such as the different interpretation of the slide by experts, or if the virus genome is integrated into the host’s chromosome and produces If the virus proteins are stopped, the staining may not be successful.
Real Time PCR, molecular method, which is done with the help of specific probe primers, or other methods such as ibolipa, which is done with the help of specific probes on cellulose strips. Due to the specificity and nature of the test, these methods have accurate accuracy in the results of the tests, and it is possible to inform the doctor and the patient, especially the colleagues of gynecologists, with which genotypes their patient is infected, so that they can take the appropriate treatment process or to check whether it is effective. Their treatment is to repeat the test every few months.
It should be mentioned that in Payvand Clinical and Specialty laboratory, the HPV diagnostic panel is performed by molecular method as well as the Pap Smear test. For more information and sampling conditions, please call 71400004.